
The long-standing practice of billing and collections is entering a new realm: revenue cycle management.
More than ever, this critical role in healthcare involves a delicate balancing act as revenue cycle leaders and their teams have to navigate a plethora of automated, regulated, and complex processes, while maintaining profitability for their organizations. And because more revenue is coming directly from patients, especially from those in high-copay or high-deductible insurance plans, revenue cycle leaders must seek new strategies for improving the financial health of their providers or hospital.
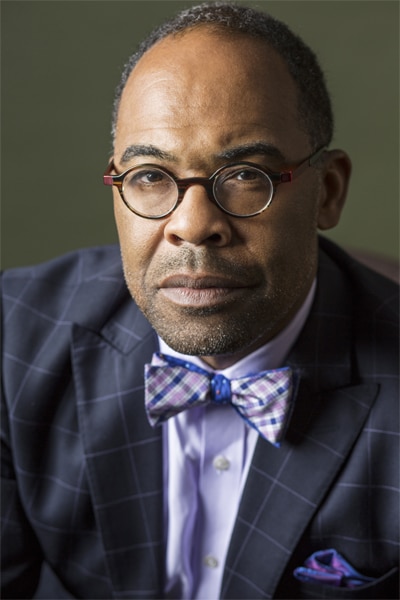
“At the end of the day, we get paid or we have to understand why we didn’t get paid,” says Fabian Stone, associate vice president for revenue cycle and health information management for Duke University Health System, a leading national academic health center in Durham, North Carolina. He oversees four departments—revenue, coding, documentation, and shares information management—along with 420 direct reports. “Revenue integrity is the safeguard to protect our assets,” he says.

Stone’s job is to protect and preserve that integrity. He says that revenue cycle teams spend money toward collecting payments from patients, educating providers on insurance policies, and appealing complex claims. But even with powerful management software and trained employees, maximizing profits can be challenging. “Revenue cycle management is facing a set of challenges that require a thoughtful approach and leadership in response to consumer and market demands,” he says. “Leaders must understand how elements of clinical delivery impact financial performance.”
“For hospitals and health systems, the shift to value-based payment demands a relentless focus on improving patient outcomes and reducing total cost of care,” says Mark Colin, vice president and general manager of 3M Health Information Systems. “Under Fabian’s leadership, Duke University Health System’s revenue cycle and health information management teams are meeting these challenges with innovative programs that safeguard revenue integrity and promote accurate outcomes data. We are proud to be Duke University Health System’s technology partner, and we look forward to our continued collaboration.”
One example of how changes in the healthcare industry have increased the importance of revenue cycle management comes from claims data, which Stone says is increasingly driving hospitals’ and physicians’ reputations. “The demand for quality measures, patient safety indicators, and patient satisfaction scores have made revenue collection about more than just collecting dollars,” he says. “Healthcare consumers rely on providers to improve their health, and healthcare providers do not turn away patients in need.”
Efficient processes for patients, providers, cash flow, and quality outcomes, he says, are contingent on incorporating a multilayered management approach, known by the acronym TECH—talent management, efficiency, cash flow, and habits.
Talent Management
The guiding principle of talent management is that people are an organization’s best resource. “Recruiting and keeping the right people for the right jobs is critical for success,” Stone says. “Revenue cycle needs people, such as medical coding analysts and clinical documentation nurses, who are active collaborators, quick learners, and sophisticated problem-solvers capable of adapting to change—these people are unicorns.”
These employees also must be able to understand large data sets to educate physicians on insurance policies for improving reimbursement. For example, coders must be able to understand standard coding practices, quality measure guidelines, and payer-specific coding rules. But the right people are just one aspect of successful revenue cycle management, Stone says.
Efficiency
Revenue cycle leaders must also worry about efficiency. Organizations can enhance their efficiency by using technology as a tool for data governance to meet the goals and objectives of customers in quantifiable terms, Stone says. Technology can be useful in assessing data collection, claims submission, account processing, and automation. “A high level of efficiency begins and ends with accountable leaders who show the ability to change at a moment’s notice,” he says. “That flexibility will ensure adherence to regulations and mitigate risks that are associated with coding, billing, and records governance.” However, talent management and efficiency aren’t useful unless an organization can maintain its bottom line.
Cash Flow
Stone says that declining revenue, tightening margins, and an increasing amount of bad debt are driving revenue cycle management teams to rethink how to stabilize cash flow and maintain profit. “Leaders must focus on understanding data from many sources, such as utilization trends, readmissions, and discharge dispositions,” he says. Also, leaders should provide stronger integration between clinical processes and denial processes—such as reviewing case types for prior authorization at scheduling, creating questionnaires at the operating room, and creating scheduling hubs, he says. This integration is essential to optimize payer relations, and it is at the core of developing policies that create a more cost-effective revenue cycle. Lastly, it’s important to step back from the nitty-gritty details and look at the bigger picture of the healthcare industry, Stone says.
Habits
Changing health policies require deeper understandings of the consumer experience to transform how a revenue cycle develops products, services, processes, and initiatives, Stone says. “This effort requires a human-centered approach for planning and implementation that guides staff toward becoming design thinkers who integrate the needs of people, the possibilities of technology, and the needs of the business together.”
Stone believes that an effective TECH leader must engage in performance monitoring and develop action plans to integrate people, processes, and technology to come up with creative solutions to interdisciplinary challenges. Above all, Stone sees technology as a unifying solution to improve an organization’s talent management, efficiency, cash flow, and habits. “Leaders must guarantee the use of technology as the critical platform for tracking, automation, and interaction,” he says. “Technology is essential to improving both clinical quality and the revenue cycle performance and enhancing workflow.”
Stone’s faith in this approach stems from a long career in healthcare. He grew up in a small town outside Durham, North Carolina, and earned a bachelor’s of science degree in medical technology at Winston-Salem State University. He worked in a lab at the University of North Carolina (UNC) Hospital for a while, then took a sabbatical to study hospital management and obtain a master’s degree in hospital and business administration from Pfeiffer University. Back at UNC Hospital, he worked on practice management before moving into coding and compliance. Eventually, he “changed colors from Tar Heel blue to Duke blue,” and worked in several areas, including clinical documentation and health information management. He was named an associate vice president in 2012.
“Healthcare today is all about change, and organizations needs leaders to manage that change,” he says. “This industry is highly regulated, and you have to mitigate all the risks that go with billing and records governance. A flexible and diverse workforce will allow you to manage change that is coming quicker and quicker.”












